The discovery and use of antibiotics is one of the most significant developments in medical history.
In its original sense, the term 'antibiotic' refers to a naturally formed metabolic product of fungi or bacteria that has a growth-inhibiting or even lethal effect on other microorganisms.
In the meantime, "antibiotics" has become established as the name of a whole group of drugs that help with bacterial infections, but not with diseases such as influenza or colds caused by viruses. Specifically, the active ingredients in these therapeutics help the body's defense system to better fight off invading pathogens.
Antibiotic manufacturing
Since the discovery of penicillin in the 19th century and its eventual invention in 1928, the number of antibiotics available has increased enormously. This is mainly due to the way they are manufactured: While the first medically applied antibiotics were natural metabolites of fungi and bacteria, they can now also be produced partially or fully synthetically.
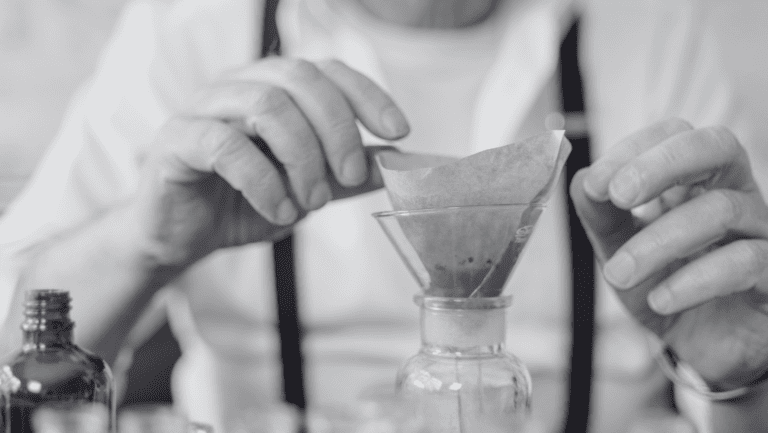
The production process requires a culture fluid, a so-called fermentation medium, on which certain fungi or bacteria can be cultivated. The antibiotic is then extracted and purified from the microorganisms. This was first achieved with penicillin by the group led by Howard Florey and Ernst Boris Chain at the University of Oxford.
Nowadays, antibiotics are available in a wide variety of forms: in addition to film-coated tablets and capsules, they can also be administered as injections or infusion solutions. In powder form, they are used to prepare a suspension for ingestion, but they can also be purchased commercially as ready-to-use syrups.
Application and mode of action of antibiotics
Since the first use of antibiotics, science has learned a lot. Because of the short half-life, i.e., the length of time a substance can act in the body before it is broken down or "eliminated," penicillins, for example, must be taken several times a day to maintain their effect - in addition, antibiotics must be taken for longer than complaints are visible.
If the body is already weakened by a viral infection, it becomes more susceptible to attack by bacteria. In individual cases, for example, bacterial pneumonia can arise from a viral infection of the respiratory tract.
In addition, some foods have a negative effect on the success of treatment with antibiotics. Alcohol consumption during intake is generally not recommended, as the combination can lead to headaches, cardiac arrhythmias, as well as nausea, vomiting and a drop in blood pressure. Some agents react on a biochemical level with the calcium from dairy products and are thus impaired in their effectiveness. Therefore, at least two hours should elapse between taking the antibiotic and consuming dairy products. The same applies to dietary supplements containing magnesium, calcium or iron.
Not every antibiotic is effective against all bacteria. Different substances are administered depending on the type of pathogen. Broad-spectrum antibiotics can fight a wide range of pathogens, which is particularly helpful when the exact infection is unknown. Narrow-spectrum antibiotics are used in the fight against specific groups of bacteria.
In addition to broad-spectrum and narrow-spectrum antibiotics, there are reserve antibiotics that should only be administered in exceptional cases when other anti-infectives have already failed due to germ resistance.
The danger posed by multi-resistant germs
Bacteria reproduce by cell division. Just as with virus cells, changes in the genetic material of bacterial cells also occur regularly in the course of cell division. These "copying errors" (also called mutations) can lead to known antibiotics no longer being effective or only being effective to a limited extent. However, bacteria can also actively adapt to external circumstances and thus develop resistance. In hospitals in particular, resistant pathogens therefore often develop and multiply.
The risk of multi-resistant pathogens is particularly high for people with previous illnesses, newborns or during operations. Even the smallest bacterial infection can be fatal. According to estimates by the Robert Koch Institute, around 400,000 to 600,000 people in Germany alone contract multi-resistant germs every year - around 15,000 die as a result. Almost half of these deaths are due solely to the ineffectiveness of known antibiotics.
The food industry also contributes to the emergence and spread of multi-resistant germs. Preventive use of antibiotics in milk or meat production can lead to the development of multi-resistant germs, which then enter the food trade via animal products. Antibiotic-resistant germs also enter the natural environment through manure and slurry spreading in livestock farming, where they develop their effects. This promotes the increase of multi-resistant bacteria in the environment and enables them to infect humans via groundwater or contaminated bathing lakes.
Another disadvantage in the use of antibiotics are potentially occurring side effects such as gastrointestinal complaints, nausea or diarrhea. Likewise, allergic reactions of the skin or fungal infections may occur. This is because antibiotics also act against bacteria, whose presence the organism needs for optimal health. Thus, such drugs should really be used only when necessary.
In addition, interactions with other medicines may occur, leading to amplification, weakening or complete failure of the mode of action. Particularly in the case of hormonal contraception, antibiotics can reduce the effectiveness of contraceptives.
Principle: antibiotic use with caution
Antibiotics have revolutionized medicine. However, around 100 years after their discovery, various antibiotics are available, but multi-resistance of bacteria is increasingly being observed, which means that many of the known antibiotics are not effective or not effective enough. At the same time, fewer and fewer new antibiotics are being developed and approved that can help against such germs. Therefore, we should all think about a conscientious and sustainable use of antibiotics, which concerns both the direct use as a medicine, but also the indirect consumption (e.g. via factory farming or industrial and production by-products discharged into the environment).